Non-communicable diseases (NCDs) are responsible for 74% of deaths worldwide. They have a tremendous impact on people’s mental and physical well-being whilst also having an economic impact through losses in productivity and unemployment. There has been an increasing demand by policymakers for tools that can evaluate both the short- and long-term effects of interventions that curb the growing burden of NCDs on health, economic and societal outcomes.
In order to meet this demand, the model simulates demographics and health-associated risk factors such as nutrient intake, physical activity, and obesity and their role in the incidence of new diseases. To our knowledge, Health-GPS is the first microsimulation tool that accounts for the role of diseases in the incidence of new diseases, such as the role of diabetes in the development of liver and pancreatic cancers. At the end of each simulation, Health-GPS produces a variety of different metrics that allow decisionmakers to assess the impact of their health-related policies on targeted populations in terms of disease prevalence, mortality, quality of life, and savings in terms of healthcare expenditures.
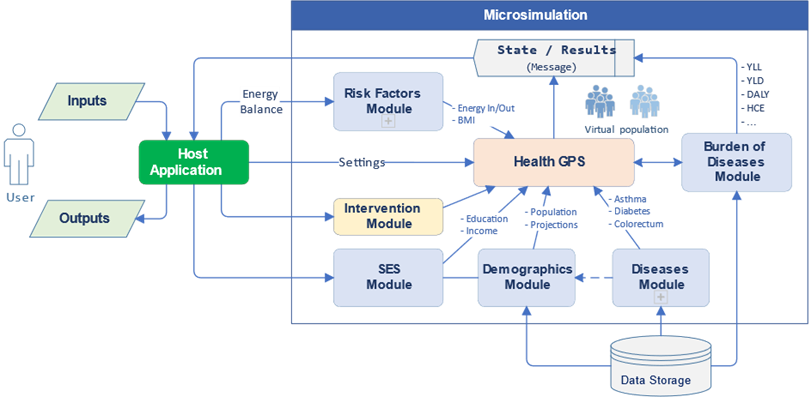
Figure 1: High-level components of the Health-GPS
Health-GPS uses mathematical models and machine learning algorithms to analyse real-world data such as national surveys. The aim is to extract the main statistical properties between variables from these surveys whilst matching estimated and projected demographic and epidemiological metrics from international databases.
To simulate the impact of health-related policies, the model is run twice. The first run, called the “baseline scenario,” simulates the status quo and reflects the evolution of the population over time in the absence of any external forces. In the second run, called the “intervention scenario,” a change, such as a marketing regulation on advertising targeting children, reflecting the impact of a health policy is applied to the targeted risk factor. This impact will subsequently be transmitted to the other risk factors, diseases, and mortality through the model equations. The difference in outcomes between the baseline and intervention scenarios is the effect of the simulated health policy (Figure 2).
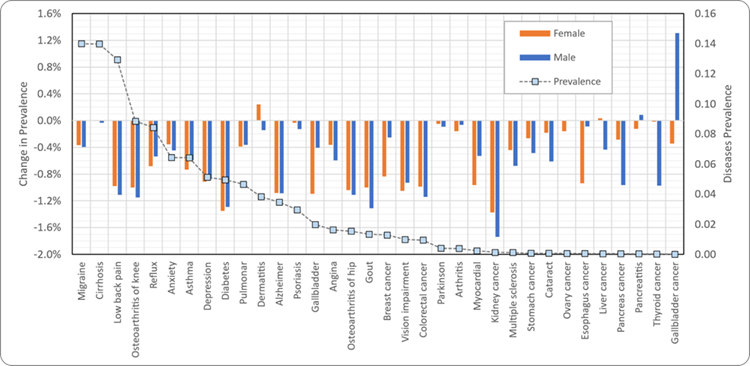
Figure 2: Percentage change in disease prevalence due to marketing restrictions in France by 2050
Health-GPS is an individual-based microsimulation implemented using modern C++20 standard and object-oriented principles and is available open source (https://github.com/imperialCHEPI/healthgps). The software provides a modular and flexible framework to allow researchers to design and test the effectiveness of health policies and interventions. The Health-GPS application is cross-platform and allows users to run the microsimulation on a range of hardware, including desktop, cloud, and high-performance computers.
The research team at Imperial College London (ICL) is currently tackling a number of challenges related to healthcare data and expanding the capabilities of Health-GPS to include a household structure and its impact on risk factors and disease prevalence. The team is also looking to expand the model capabilities through synergies with similar models.

